117
Views & Citations10
Likes & Shares
CASE REPORT
26-year-old male presented to emergency room early morning in an unconscious state with generalized seizures. He was febrile101.6 F with BP 160/110, HR 135/m. In Lorazepam was given. But he desaturated with SpO2 86% He was immediately intubated and put on mechanical ventilation. Pupils were bilaterally reactive and equal 4 mm. Dolls eye movement were normal. GCS was E1M2VT.Cardiovascular, respiratory and abdomen examination showed no abnormality. He was a worker in a restaurant, non-alcoholic, non-smoker, had no comorbidities with no history of substance abuse as per the relatives.
Only significant history was that he had early dinner previous night, went for night shift, came early around midnight and fell asleep. Had two episodes of loose stools during this period as told by his mother. Found to be disoriented and to have abnormal limb movements by the mother early morning, and was shifted to hospital.
Antiseizures mediation were stepped up with In Leviteracetam, and In Phenytoin as seizures continued with persistent tachycardia. He was shifted to the ICU from ER. In Thiamine for suspected alcoholic encephalopathy and Antibiotics and acyclovir started empirically. Meanwhile as seizures continued midazolam infusion was started for refractory status epilepticus and seizures were controlled clinically Bedside EEG done showed intermittent spikes. hence started on propofol infusion also. He passed 2 dark green stools after admission.
In view of persistent metabolic acidosis, sodium bicarbonate infusion was started. Repeat bedside EEG showed burst suppression Complete blood count, Blood sugar, serum urea, creatinine, were normal. Creatinine phosphokinase, thyroid function tests, Blood Culture, Viral Markers including HIV, CT Brain, Fundoscopy and CSF study were normal. Serological tests for Dengue, Malaria, Toxicology studies on RT Aspirate and urine routine offered no positive findings. Ketones were negative Autoimmune encephalitis panel showed no positive findings. Electrocardiogram revealed sinus tachycardia. ECHO and chest Xray revealed no abnormalities.
Arterial blood gas analysis revealed severe metabolic acidosis with mixed HAGMA and NAGMA (DELTA GAP = 0.5) Table 1.
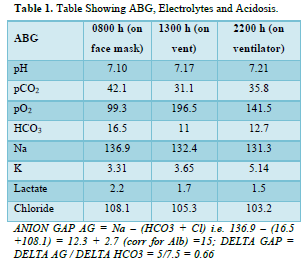
There was hypokalemia in the face of acidosis which was corrected with IV potassium supplementation Osmolar gap was 18 mOsm/kg suggesting unidentified osmoles Urine spot K /creatinine was 20 mg/gm suggesting renal losses and Urine Ph was >5.5. Urine Anion Gap could not be done.
On day 2 mechanical ventilation was continued. GCS improved with grossly preserved cranial nerve function. He was afebrile and hemodynamically stable except persistent tachycardia with no seizure recurrence and EEG showing no spikes, propofol infusion was stopped, midazolam infusion was continued. He was maintaining adequate urine output and normal blood sugar levels. RT aspiration was 900 ml in 24 h. As ABG still showed persistent metabolic acidosis In Soda Bicarbonate infusion was continued.
On day 3 MRI Brain and ultrasound abdomen was normal. With no seizure recurrence, midazolam infusion was tapered and stopped, In Levetiracetam was continued. ABG showed correction of metabolic acidosis and hence bicarbonate infusion stopped.
By day 4 patient was following commands, moving all four limbs with spontaneous eye opening and tachycardia had settled. As he tolerated SBT, he was weaned and extubated.
Post extubation the patient revealed he had consumed fish for the first time (Mackerel), at night before he fell ill.
DIAGNOSIS
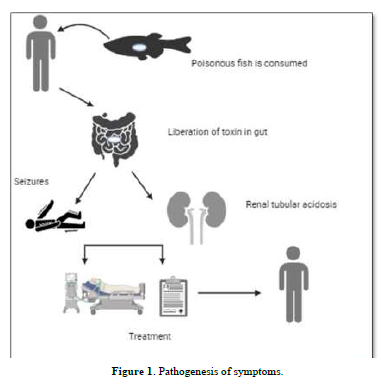
Fish Poisoning (Figure 1)
Leading to toxin mediated refractory status epilepticus and severe metabolic acidosis due to toxin induced distal renal tubular acidosis and poisoning.
DISCUSSION
Acidosis
The patient presented with severe metabolic acidosis with elevated anion gap of 5. Delta gap was < 1.0 - 0.66. Delta gap is calculated as delta anion gap / delta HCO3. In the face of elevated anion gap acidosis, a delta gap less than 1.0 indicates a mix of HAGMA and NAGMA. So, what was the cause of the acidosis. Lactate was normal, so it was not the cause. We attributed the NAGMA to Distal RTA Renal Tubular Acidosis due to the effect of toxins on the renal tubules. Drugs are a known cause and toxins are also drugging in a roundabout manner. Moreover, such toxin induced RTA has been described [1]. In Distal RTA hypokalemia, a urine pH > 5.5 and increased urine excretion in the face of hypokalemia is seen which was all present in our patient. A urine anion gap is also done at times to differentiate from extrarenal causes mainly diarrhea. However, there was no significant diarrhea. The cause of HAGMA was attributed to poisoning. Apart from lactic acidosis, ketoacidosis and uremia poisonings are the only other cause of HAGMA. The increased osmolar gap was supportive of the poisoning attributable osmoles.
Fish poisoning
Seafood poisoning is mostly due to contaminated fish which contain natural toxins and may cause illnesses if consumed. Majority of the toxins are produced by phytoplankton, a form of naturally occurring marine algae. These microalgae accumulate in the fish that are nontoxic and become poisonous fish if they feed on these algae or if they eat the other fish that have already consumed the poisonous algae [2].
Symptoms are protean and may extend from gastrointestinal problems which include nausea, vomiting, and diarrhea to Neurologic symptoms which may include numbness or tingling, pain in the joints or muscles, headaches, dizziness, and weakness as in the case of Ciguatera fish, (fish that consume algae). Mackerel belongs to Ciguatera group. Some people report that hot things feel cold or cold things feel hot. Cardiovascular problems may include irregular heart rhythm, slow (most common) or fast heart rate, and low blood pressure [3]. Amnesic, neurotoxic and paralytic shellfish poisoning from shellfish like clams, mussels and oysters are caused by diatoms (amnesic type) or dinoflagellates (neurotoxic and paralytic types) [4].
Treatment is usually supportive and symptom control. Hemodynamic support and ruling out any other potential causes of cardiovascular symptoms should be prioritized. Most patients respond to oral or intravenous hydration, correction of electrolytes, antinausea and antidiarrheal medications. Here we had a case where we had no clue to the seizures and to the refractory metabolic acidosis until the patient recovered.
Seizures Mediated by Toxins
Viewed from a physiological perspective seizure require three conditions 1. A population of pathologically excitable neurons 2. An increase in excitatory, mainly glutaminergic activity through recurrent connections in order to spread the discharge and 3. a reduction in the activity of the normally inhibitory GABAergic projections. While this remains an accepted physiology for generation of seizures, how toxins mediate seizures remains somewhat obscure. As a model of spontaneous discharges epileptic foci induced by penicillin are characterized by spontaneous interictal discharges, during which the neurons of the discharging focus exhibit large, calcium mediated paroxysmal after hyperpolarization’s [5]. Drugs like high doses of penicillin’s, carbapenems especially imipenem, levofloxacin, uremic toxins, many poisons especially organochlorides are some common causes.
- Friedman MA, Fleming LE, Fernandez M, Bienfang P, Schrank K, et al. (2008) Ciguatera fish poisoning: Treatment, prevention and management. Mar Drugs 6: 456-479.
- Goodman DM, Rogers J, Livingston EH (2013) Ciguatera Fish Poisoning. JAMA 309(24): 2608.
- Lange WR (1994) Ciguatera fish poisoning. Am Fam Physician 50: 579-584.
- Narayan R, Abdulla MC, Alungal J (2017) Transient Distal Renal Tubular Acidosis in Organophosphate Poisoning. Indian J Crit Care Med 21(3): 170-171.
- Ropper AH, Samuels MA, Klein JP, Prasad S (2019) Epilepsy Adams princioles of neurology. 18th edition New York Tata Mc Graw Hill.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Alcoholism Clinical Research
- Journal of Clinical Trials and Research (ISSN:2637-7373)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Ophthalmology Clinics and Research (ISSN:2638-115X)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)